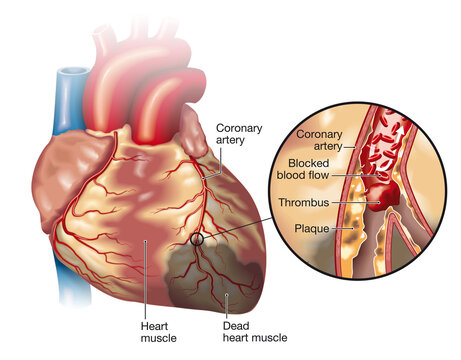
Myocardial Infarction (MI) also known as “heart attack” is due to a decreased or complete cessation of blood flow to a portion of the myocardium of the heart. simply we can say that a heart attack happens when a part of the heart muscle doesn’t get enough blood.
Myocardial infarction may be”silent,” can go undetected, or could be a catastrophic event that leads to hemodynamic deterioration and sudden death.
Before going to Management of Myocardial Infarction. Let’s learn about the assessment and nursing management of MI here.
Assessment of the patient for MI
these are the assessment to be done for Management of Myocardial Infarction
- Assessment for pain (location, intensity, radiation, frequency, aggravating factors, alleviating factors)
- Assess cardiac output, anxiety, dyspnea, level of consciousness, pallor and diaphoresis
- Assess cardiac dysrhythmias
- Asses complete vital signs
- Assess urine output, difficulty in breathing, palpitation, sweating
Nursing Diagnosis of Myocardial Infarction
- Chest discomfort due to an imbalance in oxygen demand and supply
- Decrease cardiac output related to change in frequency of heart rhythm
- Activity intolerance related to limitations imposed
- Anxiety and fear of death related to unknown disease condition
- Risk for complication related to the use of thrombolytic therapy
Management of Myocardial Infarction
- Keep the patient in complete bed rest to reduce myocardial oxygen demand, for at least 24 hours. After that mobilize slowly when the patient remains free of chest pain
- Administer oxygen by nasal cannula or face mask. Initially high flow, then 2-4 L/minute
- Relieve pain by administrating morphine sulfates as prescribed
- Administer prescribed medicine such as antiplatelet, thrombolytic therapy, beta-blockers
- Relieve patient anxiety and encourage to ventilate feelings
- Observe for side effects of medicines (bleeding from anticoagulants, bradycardia from beta blockers)
- Promote nutrition by maintaining fluid balance, low caloric with low cholesterol diet, avoiding too hot and too cold diet, salt restriction, small and frequent feeding, and encouraging a soft diet
- Promotion of regular bowel elimination. If necessary use stool softener
- Avoid straining during bowel elimination
- Maintaining enough fluid intake, and keeping a record of strict intake and output
- Change position to promote circulation and prevent pressure sore
- Maintain hygiene of the patient: mouth care, back care
- If the condition is stable, promote progressive activities (bedside mobilization, toilet mobilization)
- Provide pre-operative and post-operative care as necessary
- Preoperatively: part preparation, explanation, consent, payment, removal of ornaments, dentures, wigs
- Postoperatively: maintain airway, breathing, and circulation, watch for bleeding, provide chest physiotherapy
Discharge teaching for Myocardial Infarction
- Avoid activities that produce chest pain, extreme dyspnea, and unusual fatigue
- Weight reduction in case of obesity
- Stop cigarette and tobacco use
- Have regular exercise but do not exert more
- Avoid high-calorie and saturated fat-containing diet
- Control and maintenance of HTN, and blood sugar level


