Myocardial infarction (MI) or acute myocardial infarction (AMI), commonly known as heart attack is the interruption of blood supply to part of the heart, causing some heart cells to die. It is an irreversible damage of myocardial tissue caused by prolonged ischemia and hypoxia.
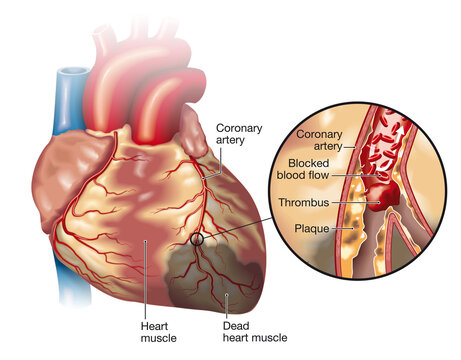
Myocardial infarction or MI is due to deprivation of blood supply to the myocardium caused by atherosclerotic plaque and subsequent occlusion of the coronary artery rupture of atherosclerotic plaque and Thrombus formation. Ischemia develops when blood flow is reduced by >80-90%
Risk Factor of Myocardial Infarction
multiple reasons and causes are there there for Heart attack. it can be divided into modifiable risk factors and nonmodifiable risk factors which are listed below
Modifiable risk factors
- Tobacco use
- High blood cholesterol
- Lack of exercise
- Obesity
- Stress
Nonmodifiable risk factors
- Family history of heart disease
- Older age
- Diabetes
- High blood pressure
what are the Causes of MI?
Multiple causes are found for myocardial infarction. some of the major causes of MI are
- Sudden narrowing or blockage of a coronary artery
- Decreased oxygen supply (acute blood loss, anemia or hypotension)
- Increased demand for oxygen ( tachycardia, ingestion of cocaine)
- Blockage of coronary artery by thrombus formation
- Intense exertion: may be psychological stress or physical exertion, especially if the exertion is more intense than the individual usually performs
- Acute severe infection, such as pneumonia can trigger MI
Pathophysiology of the Heart attack or MI
- The area of inflammation develops gradually in the coronary artery due to various causes
- Development of atherosclerosis in coronary artery
- Rupture of atherosclerotic plaque
- Obstruction or occlusion of coronary artery
- Myocardial cells are deprived of oxygen
- Ischemia develops
- Cellular injury
- Death or necrosis of cells
- Myocardial infarction
Clinical Features of MI
- Pain is the cardinal symptom of MI
- tightness, heaviness, or constriction in the chest
- some times feel like Heartburn Symptom
- Very severe and lasts longer
- Radiates to chest, throat, neck, arm, epigastrium or back
- The pain may radiate as high as the occipital area but not below the umbilicus.
- Breathlessness
- Nausea and vomiting
- Anxiety and fear of impending death
- Painless MI/ silent MI is common in the elderly and DM
Other signs
- Signs of sympathetic activation:
- Pallor, sweating, tachycardia
- Signs of impaired myocardial function
- – Hypotension, oliguria, cold peripheries, narrow pulse pressure, raised jugular venous pressure
Diagnosis of MI
- History taking
- Physical examination
- ECG (electrocardiogram): 12 lead ECG is done
- Blood test (cardiac marker test):
- Troponin
- Myoglobin
- CPK – MB
- LDH
- AST
Troponin
It is the type of protein found in heart muscle. The troponin test measures the level of troponin in the blood to help detect heart injury. Normally, troponin is almost 0 in blood, but when there is damage to the heart muscle troponin is released into the blood.
When a person has a heart attack, the level of troponin in blood elevates in the blood within 3-4 hours after injury and may remain elevated for 10 – 14 days.
Myoglobin
- It starts to rise in 1-3 hours, and peaks within 4 -12 hours
- Falls to normal within 12 hours, although many other factors increase serum myoglobin. If the serum level doubles when a second sample is drawn within 2 hours of the first sample it represents MI. if the level does not increase every two hours it excludes MI
Increased CPK – MB:
- Increased 3 – 6 hrs after the onset of MI, peak in 12 – 18 hours, and returns to normal in 3 days
LDH:
– It is plentiful in heart muscle and is released into serum when myocardial damage occurs. Serum level increases 14 – 24 hours after onset of myocardial damage, peaks within 48 – 72 hours and slowly return to normal over the next 7 – 14 days.
AST:
- It increases within several hours after onset of chest pain, peaks within 12 – 18 hours and returns to normal within 3 – 4 days.
Coronary Angiogram:
– It allows visualization of narrowing or obstructions on the coronary arteries and therapeutic measures can follow immediately.
Management of Heart Attack(MI)
It is a medical emergency that requires immediate medical attention. Treatment attempts to salvage as much myocardium as possible and to prevent further complications. Maintaining a Healthy Heart Rate should also be done.
The goal of medical management is to minimize myocardial damage, preserve myocardial functions, and prevent complications.
- Oxygen, aspirin, and nitroglycerin are usually administered as soon as possible.
- Keep the patient on complete bed rest, for at least 24 hours
- Administer high-flow oxygen in the acute phase, then at the rate of 2-4 liter, through a nasal cannula and maintain oxygen saturation level at 96 to 100 %
- Administer antiplatelet (aspirin, copilot), initially 300mg loading dose, and then continue at 75 to 150mg
- Thrombolytic therapy has been shown to improve survival rates in MI
- Thrombolytic therapy administered within the first 2 hours can occasionally abort MI and dramatically reduce the mortality rate.
- Antiplatelet agents: aspirin has been shown to reduce mortality markedly.
- Aspirin has an antiplatelet effect which inhibits the formation of further thrombi that clog arteries. Chewing is the preferred method of administration so that it can be absorbed quickly.
- Nitroglycerin: Sublingually can be given if available
- Beta-blockers: Intravenous beta blockers reduce pain, reduce arrhythmias and improve short-term mortality. Avoided if heart failure, bradycardia, or heart block
Mnemonic to recall of Management of Myocardial Infarction (MONATAS)
M: Morphine
O: Oxygen
N: Nitroglycerine
A: Aspirin
T: thrombolytic
A: Anticoagulants
S: Stool softeners
Surgical Management of MI
- Percutaneous coronary Intervention/ Percutaneous transluminal coronary angioplasty (PCI/ PTCA)
- An invasive procedure in which a balloon-tipped catheter is used to dilate the occluded coronary artery and promote – perfusion to the area that has been deprived of oxygen.
- Coronary artery stent: After PTCA, a coronary artery stent is used to prevent re-stenosis
- Coronary artery bypass graft (CABG)
In this surgical procedure, the blood vessel is grafted to the occluded coronary artery so that the blood can flow beyond the occlusion. Mostly saphenous vein is used.